The Bottom Line: “Patients with symptoms of heart failure and those with risk factors should be examined for pulmonary rales, jugular venous distention, a third heart sound, and peripheral edema and should have an ECG and chest radiograph” (Badgett)
“Very helpful findings [for detection of heart failure] are radiographic redistribution and jugular venous distention. These findings, when used alone, only help when they are abnormal and so can confirm the presence of increased filling pressure in patients with known severe systolic dysfunction. Among patients referred for consideration of cardiac transplant with a high (73%) prevalence of increased filling pressure, radiographic redistribution indicates an 80% to 90% probability and jugular venous distention, an85% to 100% probability of increased filling pressure. The absence of either finding cannot rule out increased filling pressure. In patients with lesser probabilities of increased filling pressure, such as those without known severe systolic dysfunction, isolated findings may not be useful. Somewhat helpful findings include dyspnea and abnormal vital signs. Radiographic cardiomegaly is somewhat helpful but loses its specificity after the initial detection of increased filling pressure because it can be a permanent finding and not fluctuate with changes in filling pressure. Dependent edema is helpful only when present. Edema is highly specific for increased filling pressure, although it has poor sensitivity.” (Badgett)
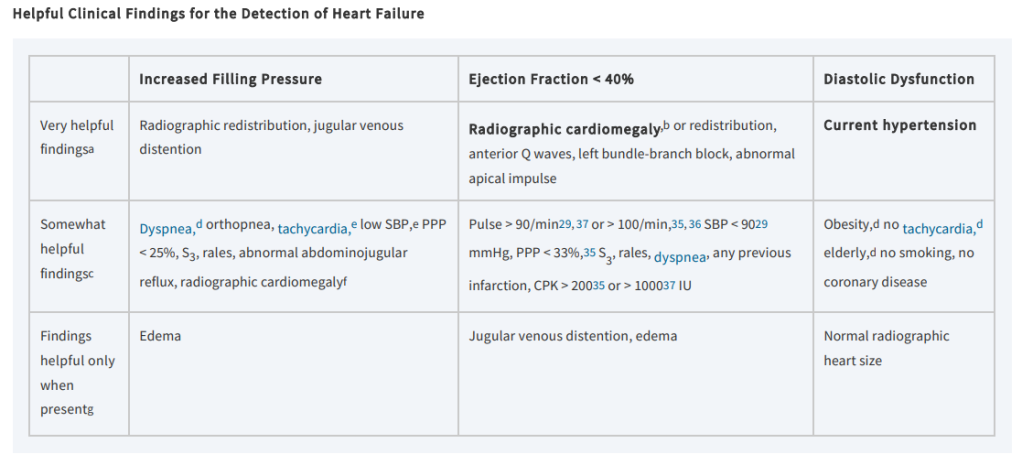
“Patients with heart failure can have decreased exercise tolerance with dyspnea, fatigue, generalized weakness, and fluid retention, with peripheral or abdominal swelling and possibly orthopnea. Patient history and physical examination are useful to evaluate for alternative or reversible causes. Nearly all patients with heart failure have dyspnea on exertion. However, heart failure accounts for only 30 percent of the causes of dyspnea in the primary care setting. The absence of dyspnea on exertion only slightly decreases the probability of systolic heart failure, and the presence of orthopnea or paroxysmal nocturnal dyspnea has a small effect in increasing the probability of heart failure (positive likelihood ratio [LR+] = 2.2 and 2.6).” (King)
Continue reading