The Bottom Line: “Lymphadenopathy is the enlargement of 1 or more lymph nodes. Patients may be alerted to the presence of enlarged lymph nodes by noticing visible nodular swelling, palpability, pain, or tenderness in 1 or more lymph node regions. It is normal to be able to palpate small lymph nodes in the neck and groin regions but generally not in the supraclavicular fossa, axilla, epitrochlear, or popliteal regions.”
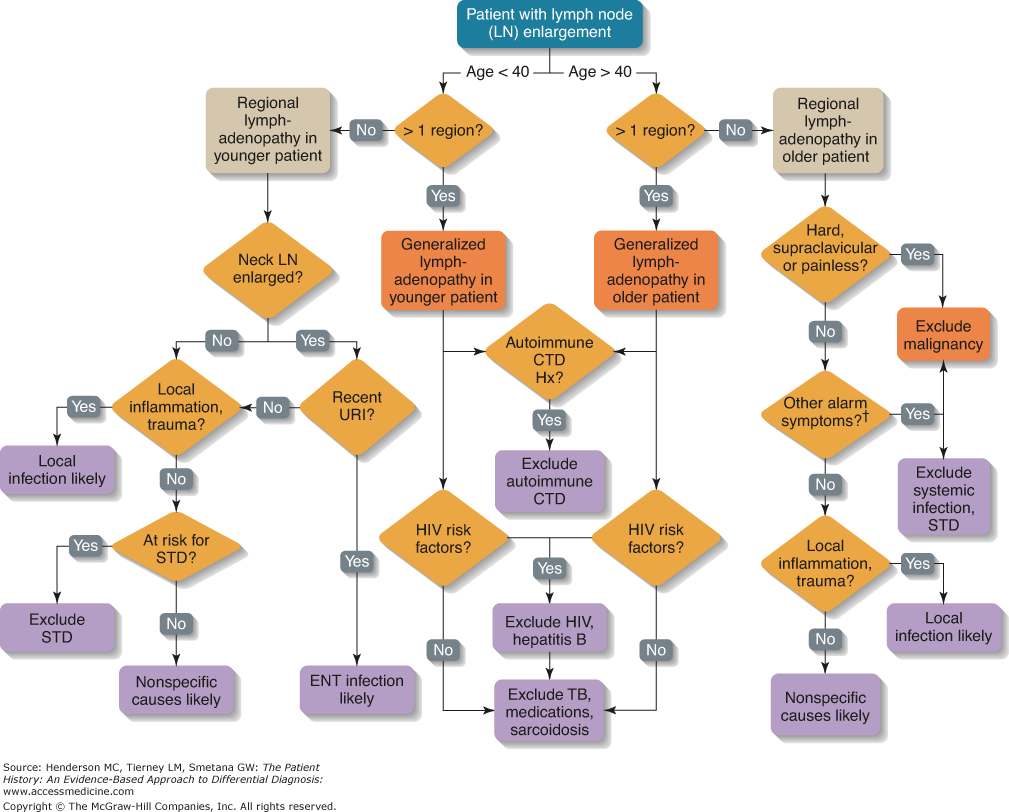
Diagnostic algorithm: “Lymphadenopathy. STD, sexually transmitted disease; CTD, connective tissue disease; Hx, history; TB, tuberculosis; URI, upper respiratory infection; ENT, ear, nose, and throat. †Other alarm symptoms suggestive of malignancy include progressive lymph node enlargement over weeks and months, alcohol and tobacco use, constitutional symptoms (malaise, fatigue, fever, unintentional weight loss, night sweats), hoarseness, dysphagia, chronic cough, hemoptysis, hematuria, hematochezia, melena, abdominal pain, and axillary or epitrochlear adenopathy without local trauma or infection.” (Zaroukian)
Evaluation
Cause of lymphadenopathy may be evident on history and physical exam alone or found incidentally in imaging. Lymph node features, as well as location (and single versus multiple nodes) of affected lymph nodes present on initial exam, may help point towards a cause.
Additional diagnostic workup may include lab tests (including blood, urine, and/or sputum), imaging, and/or biopsy.
Specific diagnostic approach is based on initial exam and clinical suspicion of cause.
